Delve into the realm of peripheral vascular disease NCLEX questions and unlock the gateway to a comprehensive understanding of this prevalent condition. This guide unveils the intricacies of PVD, empowering you with the knowledge to excel in your NCLEX exam and provide exceptional patient care.
Unravel the definition and epidemiology of PVD, gaining insights into its prevalence and risk factors. Explore the clinical manifestations, distinguishing between acute and chronic forms. Delve into diagnostic tests, deciphering the significance of physical examination, ankle-brachial index, and imaging studies.
Definition and Epidemiology
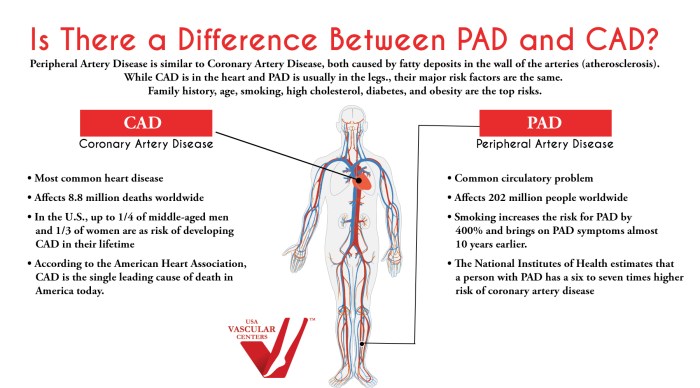
Peripheral vascular disease (PVD) refers to a group of conditions affecting the blood vessels outside the heart and brain, particularly in the legs and feet. It is a common circulatory disorder characterized by narrowing or blockage of the arteries due to the buildup of plaque, leading to reduced blood flow to the extremities.
PVD affects millions of people worldwide, with a prevalence of approximately 8-12% in adults over the age of 50. Risk factors associated with PVD include smoking, high blood pressure, high cholesterol, diabetes, obesity, and a family history of vascular disease.
Clinical Manifestations
The clinical manifestations of PVD vary depending on the severity and location of the affected blood vessels.
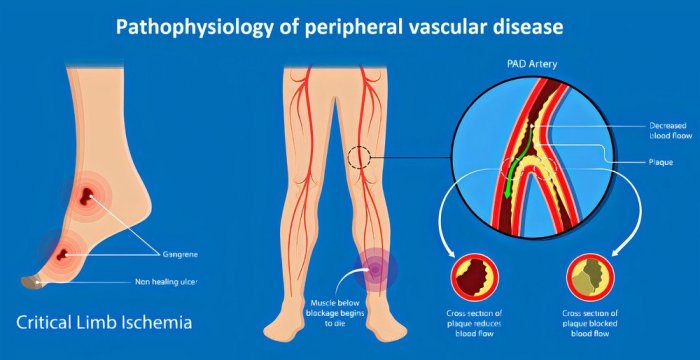
Acute PVD, also known as acute limb ischemia, occurs when there is a sudden blockage of a major artery, leading to a rapid loss of blood flow to the affected limb. Symptoms include severe pain, numbness, coldness, and discoloration of the affected extremity.
Chronic PVD, on the other hand, develops gradually over time as plaque accumulates in the arteries. Symptoms typically include:
- Leg pain or cramping that worsens with activity and improves with rest (claudication)
- Leg weakness or fatigue
- Numbness or tingling in the legs or feet
- Sores or ulcers on the legs or feet that do not heal
- Changes in skin color or temperature in the affected limb
Diagnostic Tests
The diagnosis of PVD involves a comprehensive evaluation that includes:
Physical examination:The doctor will assess the patient’s symptoms, listen for bruits (abnormal sounds) over the arteries, and check for pulses in the legs and feet.
Ankle-brachial index (ABI):This test compares the blood pressure in the ankle to the blood pressure in the arm. An ABI of less than 0.9 indicates PVD.
Imaging studies:These may include ultrasound, computed tomography angiography (CTA), or magnetic resonance angiography (MRA) to visualize the arteries and identify areas of narrowing or blockage.
Medical Management, Peripheral vascular disease nclex questions
The medical management of PVD aims to improve blood flow to the affected extremities and prevent further complications.
Pharmacological interventions:
| Drug Class | Mechanism of Action | Side Effects |
|---|---|---|
| Antiplatelet agents (e.g., aspirin, clopidogrel) | Inhibit platelet aggregation | Bleeding, gastrointestinal upset |
| Anticoagulants (e.g., warfarin, heparin) | Prevent blood clots from forming | Bleeding, bruising |
| Vasodilators (e.g., pentoxifylline, cilostazol) | Widen blood vessels | Headache, flushing, nausea |
| Statins (e.g., atorvastatin, simvastatin) | Lower cholesterol levels | Muscle pain, liver damage |
Nursing Management
Nursing interventions for patients with PVD focus on:
- Patient education:Providing information about PVD, its symptoms, risk factors, and treatment options
- Lifestyle modifications:Encouraging patients to quit smoking, manage their weight, and exercise regularly
- Wound care:Managing any ulcers or sores on the legs or feet
- Pain management:Administering pain medications and providing non-pharmacological pain relief measures
- Monitoring:Assessing the patient’s symptoms, checking pulses, and monitoring for complications
Complications
PVD can lead to several serious complications, including:
- Critical limb ischemia:A severe form of PVD that occurs when there is a complete blockage of blood flow to a limb, leading to tissue damage and possible amputation
- Amputation:The surgical removal of a limb due to severe PVD or its complications
- Heart attack or stroke:PVD is a risk factor for these cardiovascular events
Risk factors for complications include advanced age, diabetes, smoking, and poor adherence to treatment.
Preventive measures include managing risk factors, following prescribed treatment plans, and seeking medical attention promptly for any changes in symptoms.
Clarifying Questions: Peripheral Vascular Disease Nclex Questions
What is the most common symptom of PVD?
Claudication, or leg pain that occurs with activity and resolves with rest.
What is the gold standard test for diagnosing PVD?
Ankle-brachial index (ABI)
What is the most serious complication of PVD?
Critical limb ischemia, which can lead to amputation.